Who needs the PPD Skin Test Form?
The given form must be completed by a healthcare professional who is conducting a PPD skin test. A PPD skin test, also known as Manitou test, is recommended to determine whether the patient has developed an antibody response to the bacteria causing tuberculosis (TB). Whenever theManitoux test is being made, the appropriate records should be entered into this Tuberculosis Skin test Form.
What is the purpose of the TB Test Form?
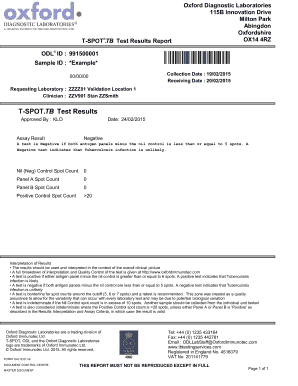
The form is used to record the results of the skin test (positive negative, induration, etc.)
Is the PPD results form accompanied by any other forms?
No, there is no need to accompany the PPD test results form by any other forms, however it should be added to the patient’s medical history and kept on file.
When is the TB test form due?
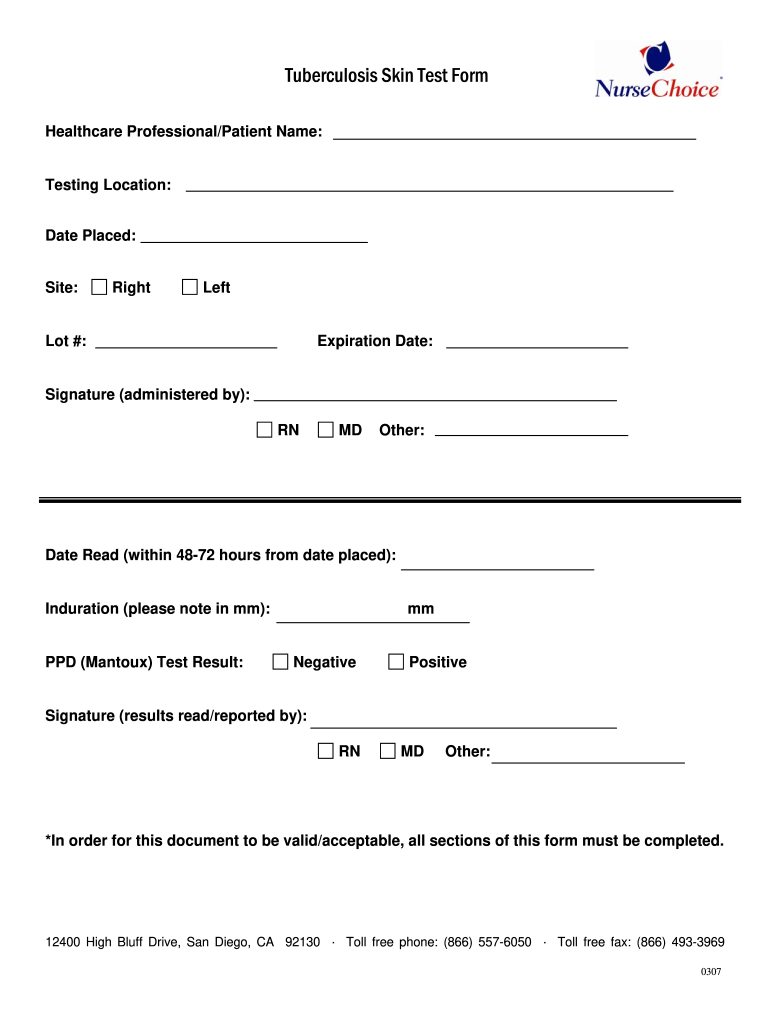
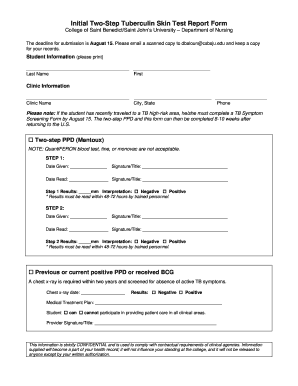
The form is not fully completed at once. The upper part of the form is to be filled out by the healthcare specialist at the moment when the injection is made. The lower part of the form is supposed to be finished in 48 to 72 hours when the patient comes the second time to receive a check-up for the reaction to the injection and find out the results.
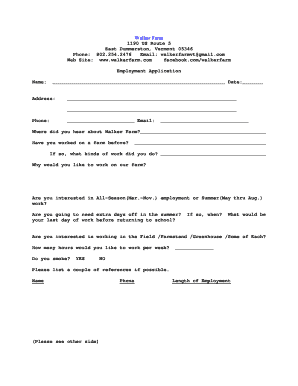
How to fill out the Tuberculosis Skin Test Form?
Besides of the result of the test, the first part form has to clearly provide all the following information:
- The name of the healthcare specialist administering the test;
- The patient’s name;
- Location of the test;
- Date when the injection is made;
- Site;
- Lot number;
- Expiration date;
- Date the result is read;
- The result (positive or negative);
- Signature of the healthcare professional in charge.
Where to send the completed Tuberculosis Skin Test Form?
The completed form should be included into the patient's medical history.